DEFINITION OF ULCER:
We can define pressure ulcers as localized areas of necrosis that tend to occur when soft tissue is compressed between two planes, one bony prominences of the patient and other external surface. Affect 9% of patients admitted to hospital and 23% of those admitted to nursing homes. The early detection and treatment accelerates recovery and reduces complications.
PATHOGENESIS:
They are produced by a prolonged and constant external pressure over a bony prominence and a hard plane, which causes ischemia of the vascular membrane, which causes vasodilation of the area (red side) fluid extravasation and cellular infiltration. If co pressure decreases, there is a strong local ischemia in the surrounding tissues, venous thrombosis and degenerative changes, leading to necrosis and ulceration.
This process can continue and reach deeper levels, with destruction of muscles, fascia, bones, blood vessels and nerves.
The forces responsible for their occurrence are:
- Pressure: is a force that acts perpendicular to the skin as a result of gravity, causing tissue crushing between two planes, one belonging to the patient and one external to it (chair, bed, probes, etc.). Pressure capillary ranges from 6 to 32 mm. Hg. A pressure greater than 32 mm. Hg., occlude the capillary blood flow in soft tissue causing hypoxia, and if not relieved, necrosis thereof.
- Friction is a force that acts parallel tangential to the skin, causing friction, or drag-motion
- Vascular Impingement External Force: Combines the effects of pressure and friction (eg Fowler position that produces sliding body, can cause friction and pressure on the sacral area).
OTHER RISK FACTORS:
These are factors that contribute to the production of ulcers and can be grouped into five main groups:
1. – Pathophysiological – Because of different health problems:
- Skin lesions: edema, dry skin, lack of elasticity.
- Disorder in oxygen transport: peripheral vascular disorders, venous stasis, cardiopulmonary disorders …
- Nutritional Deficiencies (default or excess): Thinness, malnutrition, odesidad, hypoproteinemia, dehydration ….
- Immune Disorders: Cancer, infection …….
- Altered State of Consciousness: Stupor, confusion, coma ……
- Motor impairments: paresis, paralysis …….
- Sensory Impairments: Loss of pain sensation ….
- Altered Elimination (urinary / bowel): urinary and bowel incontinence.
2. – From treatment – As a result of certain therapies or diagnostic procedures:
- Imposed Immobility resulting from certain therapeutic alternatives: Devices / appliances as casts, tractions, respirators ……….
- Treatments and Drugs having immunosuppressive action: Radiotherapy, corticosteroids, cytostatics ……
- Drilling for diagnostic and / or therapeutic: catheterization, nasogastric ……
3. – Situation – Result of changes in the personal, environmental, habits, etc..
- Immobility: related to pain, fatigue, stress …..
- Wrinkles in bedding, nightgown, pajamas, rubbing objects, etc. ..
4. – Developmental – Related to the process of maturation.
- Infants: diaper rash by …
- Elderly: Loss of skin elasticity, dry skin, restricted mobility …..
5. – Environment:
- Deterioration of the self image of the individual in the disease.
- The lack of health education to patients.
- The lack of uniform criteria in planning cures by the medical team.
- Lack or misuse prevention material, both the basic and supplementary.
- The motivation for the lack of professional training and / or specific information.
- The professional’s workload.
LOCATION – Usually in support areas that match up prominences or bone relief. The areas most at risk would be the sacral region, the heels, the ischial tuberosities and hips.
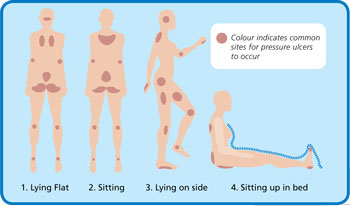
pressure ulcers locations
PREVENTING PRESSURE ULCERS:
Should be encouraged to use tables or records valuation analyzes the factors that contribute to their formation and allow us to identify patients at risk, on which to establish prevention protocols.
- The use of this table or similar, should be the first step in prevention.
- Must be comfortable, uncomplicated, including the maximum number of risk factors.
- The health care team must choose, and this must regulate their use, at admission or first contact with the patient after the deadlines set by the team.
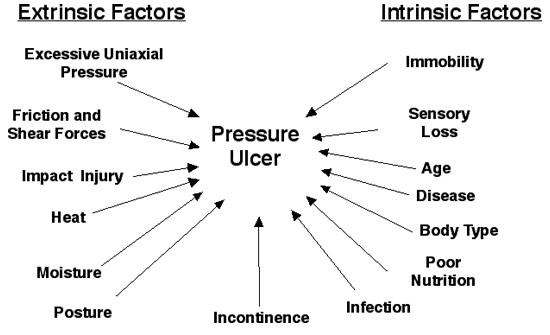
Pressure Ulcer Risk Factors
* GENERAL GUIDELINES ON PREVENTION OF PRESSURE ULCERS
Risk Assessment
- Consider all potential risk patients.
- Select and use a method of risk assessment.
- Identify risk factors.
- Record your activities and results. Evaluate.
NURSING ASPECTS
- Skin
- Examine the condition of the skin daily.
- Keep the patient’s skin at all times clean and dry.
- Use soaps or cleaning agents with low irritation potential.
- Wash skin with warm water, rinse and perform a thorough drying without friction.
- Do not use on any type of skin alcohols (rosemary, tannin, colognes, etc.).
- Apply moisturizers, ensuring complete absorption.
- Preferably use natural linen fabrics.
- To reduce potential friction injury may use protective dressings (polyurethane, hydrocolloid, …)
- Do not perform massage over bony prominences.
- Incontinence
- Treatment of incontinence.
- Reeducation of sphincters.
- Patient Care: absorbent, collectors, …
- Mobilization
- Develop a rehabilitation plan to improve mobility and patient activity.
- Perform postural changes:
- Every 2-3 hours bedridden patients, following a rotation schedule and individualized.
- In periods of sitting time demonstrations will be made if you can do it independently, teach him to mobilize every fifteen minutes.
- Maintain body alignment, weight distribution and balance.
- Avoid direct contact with each other bony prominences.
- Avoid dragging. Perform demonstrations reducing tangential forces.
- On her side, it exceeds 30 degrees.
- If necessary, raise the head of the bed as little as possible (maximum 30 °) and for the shortest duration.
- Do not use floats.
- Use devices that mitigate to the maximum pressure mattresses, cushions, pillows, local protections, etc..
- Just a supplementary material is not a substitute for mobilization.
GENERAL:
Treat those processes that can influence the development of pressure ulcers:
- Respiratory
- Circulatory disturbances
- Metabolic
- Identify and correct the various nutritional deficiencies (calories, protein, vitamins and minerals).
- Ensure adequate hydration status.
EDUCATION:
- Assess the patient’s ability to participate in the prevention program.
- Develop an education program to prevent pressure ulcers that is:
- Organized, structured and understandable.
- Aimed at all levels: patients, families, caregivers, managers, and
- Including mechanisms to assess efficiency.
TREATMENT:
Pressure ulcers are a major challenge facing healthcare professionals in their practice. Treatment of patients with pressure ulcers should include the following elements:
- Consider the patient as a whole being
- Make a special emphasis on preventive measures.
- To achieve maximum involvement of the patient and family in planning and implementation of care
- Develop clinical practice guidelines on pressure ulcers locally with the involvement of community care, specialty care and the health and social care
- Set up a framework for evidence-based clinical practice
- Make decisions based on what dimension cost / benefit
- Constantly evaluate and incorporate care practice professionals to research activities.
General guidelines on the treatment of pressure ulcers are arranged under the following headings:
- Rating
- Pressure relief in tissues
- General Care
- Ulcer Care
- Bacterial colonization and infection in pressure ulcers
- Surgical Repair of pressure ulcers
- Education and improving quality of life
- Hospice and pressure ulcers pair
- Evaluation indicators and benchmarks
1. – VALUATION:
It would be inappropriate to focus solely on the assessment of the pressure ulcer and disregard the patient global assessment.
The comprehensive patient assessment with pressure ulcers requires an assessment in three dimensions:
“Patient State”, “injury” and “your care environment.”
Initial patient 1.1 Rating
History and physical examination, with particular attention to:
- Risk factors for pressure ulcers (immobility, incontinence, nutrition, awareness, …)
- Identification of diseases that may interfere with the healing process (and collagen vascular disorders, respiratory, metabolic, immunologic, neoplastic, psychosis, depression, …)
- Advanced Age
- Toxic habits: snuff, alcohol.
- Hygiene habits and status
- Drug treatments (corticosteroids, NSAIDs, immunosuppressants, cytotoxic drugs, …
Nutritional assessment
- Use a simple tool for nutritional assessment to identify states of malnutrition (calories, protein, serum albumin, minerals, vitamins, …)
- Reassess periodically
- Psychosocial Assessment
- Examine the capacity, ability and motivation of the patient to participate in their treatment program.
1.2 Rating of the care environment
Identification of the primary caregiver
Rating attitudes, skills, knowledge and possibilities of the caregiver
(Family, informal caregivers, …)
1.3 Evaluation of the lesion
When assessing an injury, it should be able to be described by a unified parameters to facilitate communication between the different professionals involved, which in turn will allow the proper check your progress.
It is important to the assessment and registration of the injury at least once a week and whenever there are changes that suggest it.
This assessment should include at least the following parameters:
- Location of lesion
- Classification-staging
- Dimensions
- Volume
- Existence of tunelizaciones, excavations, sinus tracts.
- Meshes presents in the wound bed:
- Necrotic tissue
- Fabric gangrenous
- Granulation tissue
- Perilesional skin condition
- Integra
- Lacerated
- Macerated
- Ezcematización, cellulite, …
- Pain
- Fever
- Age of injury
- Course-evolution of the lesion
Back to nursing diagnosis Home page
2. – Relieving pressure on the tissues
Relieve pressure means preventing tissue ischemia, thereby increasing the viability and locating soft tissue injury or the optimal conditions for healing.
Each performance will be directed to reduce the degree of pressure, friction and shear.
This pressure decrease can be obtained by using techniques position (bed or sitting) and the choice of a suitable support surface.
Techniques position 2.1
2.1.1. With the patient sitting.
- When an ulcer has formed on the seating surfaces should be avoided that the individual remain seated.
- As an exceptional and always ensured that might pressure relief devices using special support this position will allow for limited periods of time, thus maintaining the good functioning of the patient.
- The sitting position of individuals that showed no injury at that level should be varied at least every hour, support facilitating change your weight every fifteen minutes by postural change or conducting drives.
- If it were possible to change the position every hour, must be sent back to bed.
2.1.2. With the patient bedridden.
- Bedridden Individuals should not rest on pressure ulcer.
- When the number of injuries, the patient’s condition or treatment goals impede the fulfillment of the above guidelines, you should decrease the exposure time or increasing the frequency of pressure changes.
- One can use a wide variety of support surfaces that can be useful in achieving this goal.
In both positions:
- Never use float or ring type devices.
- Always make a written individualized plan.
- At different levels of care, especially in the context of community care will be necessary to involve the carer in conducting activities aimed at relieving the pressure.
- For a more detailed description of these strategies is referred to the paper on General Guidelines for Prevention of Pressure Ulcers GNEAUPP
2.2. Support surfaces
The professional must consider several factors when selecting a support surface, including the patient’s clinical condition, the characteristics of the institution or the level of care and the characteristics of the surface.
The use of support surfaces is important both from the point of view of prevention, as measured from the perspective of an adjunct in the treatment of injuries put in place.
The choice of bearing surfaces should be based on their ability to counter the elements and forces that may increase the risk of these injuries or aggravate, and a combination of other values such as ease of use, maintenance, costs, and patient comfort.
The support surfaces can act at two levels, the lower the pressure surfaces, reduce levels thereof, but not necessarily the values below that prevent capillary closure.
In the case of systems of the pressure relief is a reduction of the pressure level in the soft tissues beneath the capillary occlusion pressure and eliminates the friction and shear.
It is important to remember that the bearing surfaces are a valuable ally in relieving pressure, but in no case replace the “repositioning”.
In this sense the guidelines are:
- Use a surface that reduce or relieve pressure, according to the specific needs of each patient.
- Use a static surface if the individual can assume various positions without supporting your weight on pressure ulcer.
- Use a dynamic support surface if the individual is unable to assume various positions without weight falls on the / s ulcer / s pressure.
- It is recommended that resources managers of different levels of care, both in specialized care as a community, where patients are treated with pressure ulcers or capable of suffering, the desirability of some of these areas for the benefit of its use can obtainable.
- They recommend the allocation of resources according to the patient’s risk, so it is suggested that the systematic use of a rating scale of the risk of developing pressure ulcers that are validated in the scientific literature and to suit the needs of the context reference assistance.
Requirements for support surfaces – Which is Effective in the tissue reduction or pressure relief
- – Increase the support surface
- – To Facilitate the evaporation of the moisture
- – That Heat causes the patient little
- – To reduce shear forces
- – Good cost / benefit
- – Simplicity in the maintenance and management
- – That are compatible with infection control protocols
- – Can the consistent Cardiopulmonary resuscitation needs in areas with highly complex medical patients.
Types Of Support Surfaces
- Static surfaces
- Mats-static air cushions
- Water-cushions Mattresses
- Mats-fiber pads
- Foam cushions large
- Latex Mattresses
- Mattresses-foam cushions
- Mattresses-standard cushions
- Dynamic surfaces
- Mattresses-alternating air mattresses
- Mattresses-alternating air mattress with airflow
- Beds and mattresses lateral positioning
- Fluidized beds
- Bariatric Beds
3. – GENERAL CARE
3.1. Prevent new pressure sores
- Recognizing an increased risk of developing pressure ulcers new patients who already exhibit or showed any and these lesions.
- For all this will require continued even more strongly with all the aforementioned prevention program.
3.2. Nutritional Support
- Nutrition plays an important role in the holistic approach to wound healing.
- A good nutritional support not only fovorece healing pressure ulcers but can also prevent the occurrence of these.
- An important part of the healing of these is local and occurs even with nutritional disorders, although the scientific community accepts that a poor nutritional status, a delay or inability to complete healing of the lesions and the appearance of new favors.
- Cynically severe malnutrition is diagnosed if serum albumin is less than 3.5 mg / dl, total lymphocyte count is less than 1800/mm3, or if body weight has decreased by over 15%.
- The nutritional needs of a person with pressure ulcers are increased.
The diet of patients with pressure ulcers should ensure a minimum contribution of:
- Calories (30-35 x Kq.peso Kcal / day)
- Protein (1,25 – 1,5 gr. / Kg.peso / day) (Which may be Necessary to Increase up to 2gr./Kg. Weight / day).
- Minerals: Zinc, Iron, Copper
- Vitamins: Vit C, Vit A, B Complex
- Contribution water
Should the patient’s usual diet not cover These needs Should be resorted to enteral nutrition supplements oral hyperproteic to avoid a deficiency.
3.3. Emotional Support
The Presence of a skin lesion can cause a significant change in the activities of daily living due to physical, social or emotional That can translate into a shortfall in demand for self-care and self-care Ability to Provide these.
For These pressure ulcers significant Can Have Consequences on the Individual and his family, in variables Such as Autonomy, self-image, self-esteem, etc. .. That it must be remembered this important dimension while Their care planning.
4. – ULCER CARE
A basic plan locally maintained ulcer Should Consider:
- Debridement of necrotic 1 tissue
- Wound Cleaning
- 3rd prevention and management of bacterial infection
- Choosing a product That Continually keep the ulcer bed moist and body temperature.
4.1. – Debridement
The Presence in the wound bed of necrotic tissue and eschar Either black, yellow, .. , Dry or moist nature, acts as an an ideal medium for the proliferation of bacteria and prevents it the healing process.
In any case, the overall situation of the patient condition the debridement (patients with bleeding disorders, patients in the terminal phase of illness, etc. ..)
The debrided tissue characteristics, the type of guide Equally to perform debridement.
By practice we classify methods of debridement in:
“Sharp (surgical)”, “chemical (enzymatic)”, “autolytic” and “mechanical”.
These methods are not mutually incompatible, so it would be advisable to combine them for best results.
4.1.1. – Sharp or surgical debridement
He is Considered as the fastest way to remove areas of dry eschar adherent to deeper or wet necrotic tissue Levels. Surgical debridement is an invasive procedure That Requires knowledge, skill and technique and sterile equipment. Moreover, the policy of each institution to determine level of care performed by Whom and where.
Sharp debridement must be in different plans and session (unless radical surgical debridement), always starting from the central area, seeking to Achieve early release of devitalized tissue on one side of the lesion.
Given the Possibility of the onset of pain In This technique, it is advisable Applying an analgesic t6pico (2% lidocaine gel, etc..).
Bleeding can be a common complication Control That Can Usually by direct compression, hemostatic dressings, etc. .. If you did not give The Situation With The above Measures will be used to suture the bleeding vessel.
After controlling the bleeding would be advisable to use for a period of 8 to 24 hours to dry dressing, changing later by a wet dressing.
4.1.2. – Debridement chemical (enzymatic)
Chemical or enzymatic debridement is a method to Assess When the patient does not tolerate surgical debridement and no signs of infection.
There are several products on the market enzymatic (proteolytic, fibrinolytic, …) Which can be used as agents of chemical debridement of necrotic tissue.
Collagenase is an example of this type of substances.
There is scientific evidence indicating it favors the growth That debridement and granulation tissue.
Intended to be used When, it is advisable to protect the skin by periulceral zinc paste, siliciona, etc. As well, to Increase the level of moisture in the wound to potentiate Their action.
4.1.3. – Autolytic debridement
Favored by debridement Autolytic be using products designed on the principle of wet cure.
It is produced by the combination of three factors, hydration ulcer bed, fibrinolysis and the action of endogenous enzymes on devitalized tissue.
This formulation is more selective debridement and atraumatic, Requiring no specific clinical skills and being well accepted Generally by the patient.
It has a slower action in time. Any dressing can produce moist healing conditions, in general and in hydrogels espec?ficamente amorphous structure are capable of producing products autolytic debridement.
For gangrenous tissue wounds, amorphous structure in hydrogels (gels), for its moisturizing Facilitate removal of non-viable tissues and Should Be Considered THEREFORE debridement as one option
4 1.4. – Mechanical debridement.
It is a traumatic and non-selective technique.
Mainly by mechanical abrasion is performed by friction forces (friction) dextran?meros use by the pressurized irrigation of the wound or the dressing moistened Which dries utilizaci6n past 4-6 hours adhere to the necrotic tissue, but Also the woven healthy, Which Starts with removal. There are now obsolete techniques.
4.2. – Debridement
- Clean the injury INITIALLY and every cure.
- Use as standard saline.
- Use minimum mechanical force to clean the ulcer and for subsequent drying.
- Use a pressure washing to Facilitate Effective drag of detritus, bacteria and traces of previous cures but, unable to produce healthy tissue trauma.
- The most Effective washing is provided by pressure or gravity for example through Which carry a 35 ml syringe with a needle of 0.9 mm catheter Projected onto the wound saline at a pressure of 2 kg ./cm2.
- The washing pressure ulcer Between Effective and safe ranges I and 4 kg/cm2.
- Can not clean the wound Local antiseptic (povidone iodine, chlorhexidine, hydrogen peroxide, acetic acid, hypochlorite solution,) or skin cleansers.
- All are cytotoxic chemicals for the new tissue and in some cases can cause problems Their use for systemic absorption into the body.
4.3.-prevention and management of bacterial infection (see chap. 5 «The bacterial colonization and infection in pressure ulcers)
4.4.-Choice of dressing
The available scientific evidence demonstrating the clinical effectiveness and low cost optics / benefit (spacing cures, handling minor injuries …,) of the technique of wound healing in a moist environment versus traditional or cure.
An ideal dressing should be biocompatible, protect the wound from external physical, chemical and bacterial maintain continuously ulcer bed and surrounding skin damp dry and remove exudate and necrotic tissue control by absorption, leaving minimal residues in the lesion, be adaptable to difficult locations and be easy to apply and remove.
Gauze dressings can not meet most of the above requirements.
“The selection of a oposit? of moist wound healing must take place in the following variables”:
- Location of lesion
- Stadium
- Ulcer Severity
- Exudate
- Presence of canalization
- Perilesional skin condition
- Signs of infection
- General condition of the patient
- Level of care and resource availability
- Cost-effectiveness
- Ease of application in contexts of self
To prevent the formation of abscesses or ‘closure false’ injury, will need to fill in part (between half and three quarters) and tunelizaciones cavities with products based on the principle of moist cure.
The frequency of dressing change every couple will be determined the specific characteristics of the selected product.
Choose the dressing will be needed to allow optimum handling of exudate without allowing desiccate the ulcer bed or periulceral tissue injury
Moist healing dressings based on:
- Alginates: plate, tape
- Hydrocolloids: plate, granules, paste (combined with calcium alginate fiber
- – Hydrogels: plaque, in amorphous structure (gels)
- – Polyurethanes: in film / film, hydrophilic (Foam) hydrocellular plate, for cavity hydrocellular, polymer foams, polyurethane foam gel
4.5. – Adjuvant
At present the electrical stimulation is the only adjuvant therapy with complementary features enough to justify the recommendation. May be brought in ulcers pair stage III and IV pressure who have not responded to conventional therapy. In any case you should make sure that you have the right equipment and personnel trained in their use, following the protocols that have demonstrated safety and efficacy in controlled trials.
5. – Colonization and bacterial infection in pressure ulcers
All pressure ulcers are contaminated by bacteria, which is not to say that injuries are infected.
In most cases a precludes effective cleaning and debridement that bacterial colonization progressing to clinical infection.
Diagnosis of infection associated with pressure ulcer should be mainly clinical.
The classic symptoms of local infection of the skin ulcer are:
- Inflammation (erythema, edema, tumor, heat)
- Pain
- Odor
- Purulent exudate
Infection of an ulcer may be influenced by factors specific to the patient (nutritional deficiency, obesity, drugs, immunosuppressants, cytotoxic, concomitant diseases, diabetes, cancers, …, advanced age, incontinence, etc..) And other injury-related (stage , presence of necrotic tissue and gangrenous, canalization unstressed injuries, poor circulation in the area, etc. ..)
In the presence of signs of local infection should be intensified cleaning and debridement.
If, within two to four weeks, the ulcer is not progressing well and continuing with signs of local infection, having ruled out the presence of osteomyelitis., Cellulitis or sepsis, should be implemented a treatment regimen with a local antibiotic effective against microorganisms most frequently infected pressure ulcers (eg silver sulfadiazine, fusidic acid …) and for a maximum period of two weeks.
If the injury does not respond to local treatment, shall be then, bacterial cultures, qualitative and quantitative, preferably by percutaneous aspiration needle biopsy tissue, avoiding, if possible, by collecting exudate smears can detect only surface contaminants and not true microorganism responsible for the infection.
Identified the germ will pose specific antibiotic therapy, reevaluate the patient and injury.
- Infection control.
- Follow precautions body substance isolation
- Use clean gloves and change them every patient
- Hand washing between procedures with patients is essential.
- In several patients can ulcers, start with the least contaminated
- Use sterile instruments surgical debridement of pressure ulcers
- Do not use Local Antiseptics.
- Should be Administered Systemic antibiotics prescription low patients with bacteremia, sepsis, advancing cellulitis or osteomyelitis.
- Meet Regulations for disposal of your institution.
6. – Surgical repair of pressure ulcers
Should be Considered surgical repair in patients with pressure ulcers stage III or IV unresponsive to conventional treatment.
Similarly, like elements will be Necessary to Assess the quality of life, risk of relapse, patient preferences, and so on.
Along with the potential to be a candidate for surgery (postoperative immobility Affected Avoiding pressure on the region, adequate nutrition, medically stable patients, etc.).
7. – EDUCATION AND IMPROVING THE QUALITY OF LIFE
The education program must be an integrated part of quality improvement.
Educational programs are an essential component of the care of pressure ulcers.
These integrate basic knowledge Should About these injuries and Should cover the full spectrum of care for prevention and treatment.
Will be Directed Toward patients, families, caregivers and health professionals.
8. – Palliative Care and Pressure Ulcers
The patient is an end stage of the disease it has been Justified by claudicaren order to avoid the occurrence of pressure sores. In the event the patient develops That Should pressure ulcers act:
No blaming the care environment appearance of the lesions.
It is a common complication and Often at That stage, probably inevitable.
Posing realistic therapeutic goals According To the possibilities of healing, Avoiding the possible aggressive techniques.
Keeping the wound clean and protected to Prevent the infection development.
That Dressings Selecting the frequency distance allow cures to avoid the discomfort Caused by This procedure.
Improving patient comfort, Avoiding pain and trying to control, if any, the smell of lesions (by activated charcoal dressings, metronidazole gel, etc. ..)
In agony situation will be Necessary to Assess the need for repositioning the patient.
9. – Evaluation: Indicators and parameters
The evaluation process is a basic tool for Improving the Effectiveness of the Procedures used in the care of pressure ulcers.
It is Necessary to Establish a quality program With The goal of Improving the care provided to patients, Facilitate and enable teamwork objectify clinical practice.
The problem of These lesions Should be Approached from an interdisciplinary approach.
The results of the care can be Measured based on the Incidence and Prevalence of pressure ulcers.
The Incidence and Prevalence studies Periodically Should be performed to monitor them and integrate them happen ideality into a local policy on pressure ulcers.
As a Tool to Assess the evolution of These injuries can be used severity index.
Other descriptive variables can be used while Evaluating the process. Related to the injury (staging, number of injuries, age, volume, origin etc.) Or Referred the patient (age, sex, risk assessment scale for pressure ulcers etc.).
Prevalence = Number of patients with pressure ulcers divided by the overall number of patients to study at That Time.
Incidence = Number of pressure ulcers in patients Developing GIVEN period divided by the overall number of patients Studied During That period
Severity index (Braden B) = (length + width) divided by 2] x stage of the UPP.
CONCLUSIONS:
Pressure ulcers can and Should be avoided with good nursing care That Within an overall plan includes multidisciplinary work of the physician, nurse / or patient and family. Must find the perfect treat